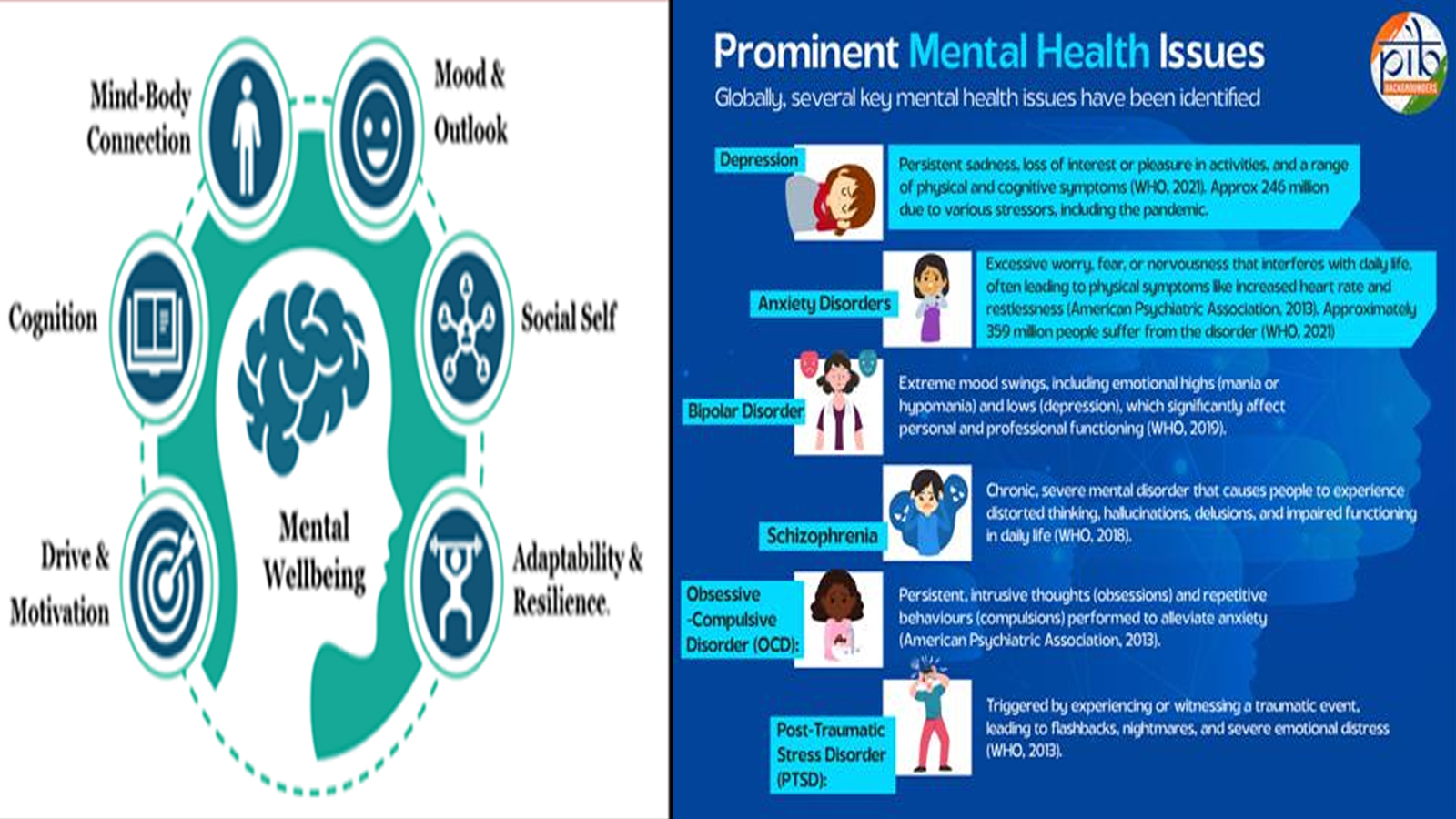
Mental well-being is not merely about feeling happy or stress-free – it’s about the ability to think, feel, connect, and function effectively in daily life. In recent years, global and national attention on mental health has surged, transforming what was once a silent struggle into a central conversation about human rights, public health, and social development.
According to the World Health Organization (WHO), mental health conditions are among the leading causes of disability worldwide. An estimated 1 in 7 people globally – more than 1.1 billion individuals – live with a mental disorder. In India, the National Institute of Mental Health and Neurosciences (NIMHANS) estimates that about 11 in 100 people suffer from some form of mental illness.
The burden of mental illness is profound. Disorders such as depression and anxiety account for a significant share of “years lived with disability” (YLD) across all age groups, especially among people aged 15 to 29. The Lancet (2020) estimated that mental health disorders contribute to 5.2% of the global disease burden, underscoring their growing impact on health systems and economies worldwide.
The Indian Context: A Nation Confronts Its Mental Health Crisis
India’s National Mental Health Survey (2015-16) revealed that 10.6% of Indian adults – roughly 11 in every 100 – live with a diagnosable mental disorder. The lifetime prevalence stands at 13.7%, with urban areas (13.5%) reporting higher rates than rural regions (6.9%).
Mental health challenges are notably higher among women, with 20% of Indian women experiencing issues like depression and anxiety, compared to 10% of men.
The country also faces a growing suicide crisis. The National Crime Records Bureau (NCRB) reported 171,418 suicides in 2023, with men accounting for nearly 73% of the total.
Despite the scale of the problem, access to treatment remains limited. The NIMHANS survey found that 70% to 92% of people with mental disorders do not receive proper care, largely due to stigma, lack of awareness, and a shortage of trained professionals. India has only 0.75 psychiatrists per 100,000 people, far below the WHO’s recommended minimum of 3.
The Costs of Neglect: Health, Economic, and Social Consequences
Poor mental health is deeply intertwined with physical and economic outcomes. Individuals with depression face a 72% higher risk of developing cardiovascular disease, according to The Lancet Psychiatry (2025). Chronic pain and sleep disturbances are also more common among those struggling with mental health issues.
Economically, the consequences are staggering. The WHO estimates that depression and anxiety cost the global economy $1 trillion annually in lost productivity. By 2030, the overall global financial burden of mental health conditions – including healthcare and indirect costs – is projected to reach $16 trillion.
Beyond economics, mental health challenges often lead to social isolation, strained relationships, and stigma. In low- and middle-income countries, stigma remains one of the greatest barriers to care, trapping individuals in cycles of shame and silence.
A Growing Crisis Among the Young
Half of all mental health conditions begin by age 14, and three-quarters by age 24, according to WHO data. The Lancet (2017) highlighted how untreated mental health issues in adolescence are linked to poor academic outcomes, substance abuse, and self-harm. The COVID-19 pandemic has only deepened these challenges, with global rates of anxiety and depression rising by nearly 25%.
Global Frameworks: A Shift Toward Inclusion and Access
The WHO’s Comprehensive Mental Health Action Plan (2013–2030) urges countries to strengthen leadership, integrate mental health into community-based care, and promote preventive strategies. Its 2022 World Mental Health Report called for transformative action – to value mental health, reshape environments, and move from institutional to community-based models of care.
India’s Expanding Mental Health Agenda
India has made significant strides in recent decades, moving from isolated psychiatric care to a more integrated, community-based approach.
National Mental Health Programme (NMHP) – 1982
Launched to integrate mental healthcare into general health services, focusing on accessibility for vulnerable populations.
District Mental Health Programme (DMHP) – 1996
Now covering 767 districts, the DMHP provides outpatient treatment, counselling, suicide prevention, and awareness programmes through community-based teams of psychiatrists, psychologists, and nurses.
National Suicide Prevention Strategy (NSPS) – 2022
Targets a 10% reduction in suicide mortality by 2030, with initiatives such as school mental health screenings, helplines, and workplace wellness programmes.
Building Capacity: Training, Technology, and Infrastructure
India currently operates 47 government mental hospitals, including premier institutions like NIMHANS (Bengaluru), LGBRIMH (Tezpur), and CIP (Ranchi).
Under the Manpower Development Schemes, 25 Centres of Excellence and 47 postgraduate departments have been strengthened to produce more psychiatrists, psychologists, and psychiatric social workers.
Digital platforms are also revolutionising outreach. The Digital Academies launched in 2018 have trained over 1.76 lakh health professionals, while the iGOT-Diksha platform has enhanced mental health capacity among frontline workers.
Ayushman Bharat and the Rise of Digital Mental Healthcare
A major milestone in India’s mental health reform is the integration of mental health services into Ayushman Arogya Mandirs under Ayushman Bharat.
Over 1.75 lakh primary and sub-health centres now provide mental healthcare as part of comprehensive primary health services.
The Ayushman Bharat-Pradhan Mantri Jan Arogya Yojana (PM-JAY) also offers cashless treatment coverage of up to ₹5 lakh per family annually, including treatment for 22 mental health disorders such as schizophrenia and autism spectrum disorders.
The Tele MANAS (Tele Mental Health Assistance and Networking Across States) initiative, launched on World Mental Health Day 2022, has handled over 28 lakh calls across 36 states and union territories. Its mobile app, equipped with self-care resources and video consultations, has expanded access to remote counselling and psychiatric care.
The initiative has received recognition from the WHO as an innovative model for delivering scalable and affordable mental healthcare.
A Renewed National Commitment
The Economic Survey 2024-25 identified mental well-being as a cornerstone of India’s human capital development, urging a “whole-of-community” approach. It recommended:
* Integrating mental health education in schools
* Enhancing workplace mental health policies
* Scaling up AI-powered digital mental health solutions
The Road Ahead
India’s mental health journey reflects both progress and challenges. While initiatives like Tele MANAS, Ayushman Bharat, and the District Mental Health Programme have significantly expanded access, treatment gaps and stigma persist.
Experts agree that sustained investment, awareness, and integration of digital innovation are key to building a mentally healthier society. As the WHO reminds us, “There is no health without mental health.”